What if you had a serious health condition that is common and treatable, but every healthcare provider you saw blamed you for having it?
And what if your condition put you at risk for serious diseases such as cancer, diabetes, and heart disease, but your insurance wouldn’t cover the medical appointments, medications, or surgery needed to get it under control?
That’s what it’s like for millions of Americans with obesity when they visit their healthcare professionals seeking help.
Healthcare professionals don’t blame people for having cancer, or for recurrences, yet those with obesity are often blamed for their diagnosis and failed treatments.
As a medical weight loss specialist, I see how this discrimination hurts people in tragic ways. I want to share the facts about why it happens. And close with a few simple—but powerful—steps you can take to stop the discrimination and improve access to effective obesity treatment.
Is Excess Weight Really a Personal Failing?
There is a false—but pervasive—belief that obesity is the result of overeating and inactivity. It is commonly viewed as a moral failing, rather than a treatable health condition. Those with obesity are frequently seen as lazy, unmotivated, lacking in self-discipline, less competent, non-compliant, and sloppy.
This misunderstanding has fostered a culture of blame that has not solved the problem.
Science tells a different story…
Obesity is a chronic health condition that needs to be treated as seriously as other chronic diseases such as diabetes, cancer, and heart disease. It contributes to the development of over 200 health conditions and 20 types of cancer. There are numerous contributing factors, some of which are not under a person’s control.
It requires skillful evaluation, effective treatments, and ongoing follow-up. Like other chronic conditions, it is progressive and worsens without treatment. Relapses are common.
Despite solid science, those with obesity are often stigmatized and discriminated against in every arena—the workplace, school, personal relationships, social interactions, and healthcare settings.
According to the Obesity Action Coalition, “Obesity stigma is a major issue and is the last socially acceptable form of discrimination in our society.”
The Pervasive Bias & Accepted Discrimination in Healthcare
People with obesity report that they frequently experience negative bias, stigmatization, and discrimination in healthcare settings.
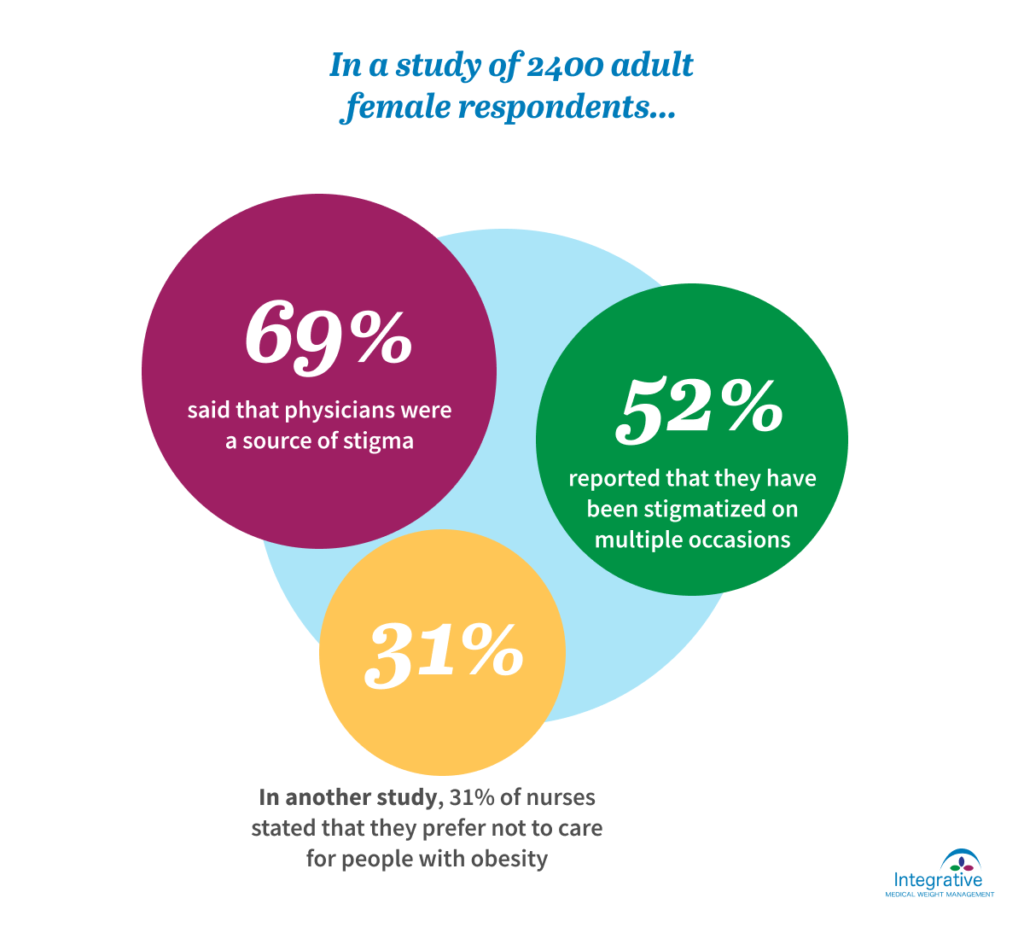
In a study of 2400 adult female respondents, 69% said that physicians were a source of stigma, with 52% reporting that they have been stigmatized on multiple occasions. Nurses also have discriminatory attitudes. In one study, 31% of nurses stated that they prefer not to care for people with obesity.
This translates into discrimination that negatively impacts the health of those affected. Research shows that when seeing people with obesity, healthcare professionals:
- Spend less time & engage in less discussion
- Are more reluctant to provide preventive health screenings
- Perform fewer interventions
- Attribute unrelated problems to weight
Like many who experience discrimination, people with obesity internalize the stigma and blame themselves for their condition. When they eat healthfully and exercise, but don’t lose weight, they conclude that they aren’t trying hard enough. Out of fear of being blamed, they don’t discuss their struggles or seek guidance from their healthcare professionals.
Research shows that internalized weight bias isn’t just unpleasant, it negatively affects physical and emotional health, increases cardio-metabolic risk, and shortens lifespan.
Are Healthcare Professionals Really to Blame?
Physicians, nurse practitioners, physician’s assistants, and other healthcare professionals don’t set out to treat those with obesity differently than other patients. They are functioning within a system—and a society—that does not provide them with key knowledge and support.
Few receive education about obesity in their foundational and continuing education programs. They are expected to be medical experts, yet have very limited knowledge about obesity and weight loss. Most do not have colleagues to teach, mentor, and support them. They work in systems with high productivity demands that don’t allow for the time needed to address the complexities involved. And when they do take the time, they are rarely reimbursed for their services.
Without evidence-based knowledge, they are not able to view their patients’ excess weight as a medical problem. Out of frustration, many fall into the trap of blaming their patients for their condition…and their failure to improve.
This results in:
- Reluctance of both clinicians and patients to initiate discussions about weight
- Patients canceling or delaying medical appointments, including preventive screenings.
- Health outcomes that are less favorable
- Lower likelihood of maintaining weight loss
The Ultimate Barrier: Insurance Coverage
Despite the challenges obesity presents, effective treatment is available. Professional guidelines recommend a comprehensive approach that includes nutritional therapy, physical activity prescriptions, stress reduction, and sleep promotion, as well as anti-obesity medications, and for some, surgery.
For those who are fortunate enough to find a healthcare professional that offers effective treatment, the chance of insurance coverage is low. And when services are covered, it is typically limited to a few visits per year. Given the serious nature of weight issues and the complexities involved, this is not adequate.
Despite their effectiveness—and FDA approval—anti-obesity medications are rarely covered by insurance. Without coverage, the majority of approved medications are cost-prohibitive for most people. When they are covered, there is a cumbersome pre-authorization process that requires the participation of both clinician and patient. And after jumping through numerous time-consuming hoops, approval is often denied. It is tragic when we find something that works, but can’t use it because there is no insurance coverage.
If you think this is discriminatory, you are right.
If you think this is unfair, you are right.
If you think this is short-sighted, you are right.
If this were happening for cancer or heart disease or high blood pressure, people would be marching in the streets!
How Do We Solve This Problem?
We need an army of knowledgeable healthcare providers, a bevy of policymakers, and an infantry of informed citizens to reverse course.
The fact that 39.8% of U.S. adults have obesity and another 33% fall into the overweight category makes this important to all of us. With growing prevalence and severity, more Americans are at risk of becoming sicker—and ultimately incapacitated—by the complications of excess weight.
It is imperative that we work towards finding effective solutions for this public health crisis. The health and financial consequences of not doing so are high for those affected, and for society itself.
We need to replace myths with facts, bias with science, and stigma with respect. We need to question our assumptions, expand our thinking, and start a productive dialogue. We need to illuminate and remove barriers. We need to talk about the disease, not the person.
We need everyone—business and community leaders, policymakers, clinicians, and healthcare consumers to understand the ramifications and lobby for access to effective treatment.
We Are Moving Forward
There are a number of organizations and consortiums that are doing just that. By working together, they are bringing about change in legislation, medical education, and public awareness.
During the week of October 30th, over 50 advocates from these organizations were on Capitol Hill. They visited 70 congressional offices lobbying legislators to support the Treat & Reduce Obesity Act (TROA) and recognize National Obesity Care Week.
This advocacy proved fruitful.
The U.S. Senate unanimously passed a bill designating October 29-November 4, 2017 as National Obesity Care Week.
And several legislators offered their support of TROA, bringing the total to 135 House and Senate co-sponsors. More are needed, but this is an increase of 32 since August.
You Can Make a Difference
Five minutes of your time could make a big difference for the over 90 million US adults with obesity. Below I have outlined two simple acts that could change the course of history.
Action Step 1: Contact your legislators about the Treat & Reduce Obesity Act (TROA).
This bill will expand Medicare coverage for obesity treatment, including Part D coverage for anti-obesity medications. When this bill passes, it will be a giant step forward for obesity treatment. Precedent has been that when Medicare opts to cover treatments, other insurers follow suit.
Click here to contact your legislators »
Action Step 2: Join the Obesity Action Coalition (OAC).
This 58,000 members non-profit organization is focused on education, advocacy, and support for those with obesity. Membership is open to everyone at a cost of $10. As a member, you will receive a monthly e-newsletter, updates on advocacy efforts, and a subscription to OAC’s publication, Your Weight Matters.
Better Days Lie Ahead
Let’s imagine a day in the not too distant future when those with obesity visit their healthcare providers and receive expert care delivered with warmth and respect. Their insurance covers the visits, medications, and other necessary treatments. Period. And their health improves.
If you want to learn more about the barriers and perspectives of people with obesity, healthcare professionals, and employers, click here to read about the recently published ACTION study.



